Can Psychedelics Extend Your Lifespan? What the Research Says

By Brent | Last Updated: February 5th, 2026
Can Psychedelics Extend Your Lifespan? What the Research Says
Key Takeaways
> Psychedelics show strong evidence for treating PTSD, depression, and trauma-related disorders, conditions linked to accelerated biological aging and reduced lifespan
> PTSD is associated with a 32-47% increased mortality risk, making effective treatment a longevity intervention
> Psilocybin increases neuroplasticity, which may protect against cognitive aging and support healthspan
> Evidence for direct lifespan extension is limited, but indirect longevity effects through improved mental health are plausible
> Legal, ethical, and safety considerations remain central to responsible use
The Psychedelic Renaissance Meets Longevity Science
After decades of prohibition, psychedelic research has re-entered mainstream science. Institutions once hesitant to touch these compounds are now publishing rigorous clinical trials, many focused on treatment-resistant mental health conditions.
Veterans suffering from PTSD have been central to this resurgence. Their outcomes have forced regulators, clinicians, and policymakers to reconsider psychedelics not as recreational drugs, but as powerful tools for mental repair. As this research expands, scientists are asking a broader question: if psychedelics restore mental health and adaptability, could they also support longevity?
The FDA has granted breakthrough therapy designations to both psilocybin (for treatment-resistant depression) and MDMA (for PTSD), signaling regulatory recognition of their therapeutic potential. A 2024 Phase 2 study published in the Journal of Psychopharmacology demonstrated that a single 25mg dose of psilocybin was well-tolerated in PTSD patients, with symptom improvements lasting at least 12 weeks.
For those exploring the intersection of mental and physical health optimization, understanding why longevity matters provides essential context for this emerging field.
What Are Psychedelics?
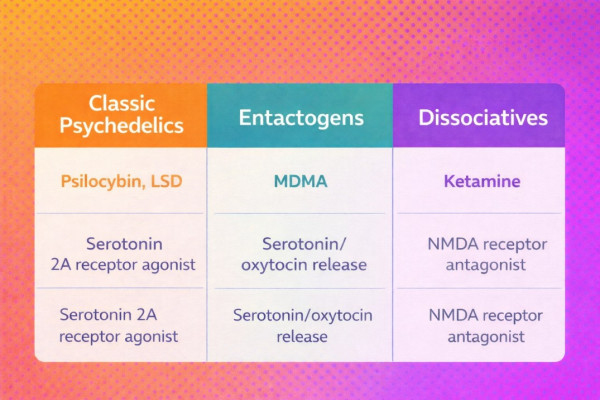
Psychedelics are compounds that alter perception, cognition, and emotional processing by acting on serotonin and related neural pathways. They include both synthesized compounds (such as MDMA and ketamine) and naturally derived substances (such as psilocybin, ibogaine, and ayahuasca).
Historically used in indigenous cultures for healing and spiritual purposes, these compounds were later stigmatized and criminalized. Modern research is now re-examining their therapeutic potential under controlled conditions.
The distinction matters for longevity applications: different compounds work through different mechanisms and may offer varying benefits for brain health and psychological resilience. For a deeper understanding of how peptides and other compounds are being explored in longevity medicine, see our comprehensive guide.
What Is PTSD, and Why Does It Matter for Longevity?
Post-traumatic stress disorder has existed as long as warfare itself. While its name has changed over time, the core symptoms, hypervigilance, emotional numbing, sleep disruption, and intrusive memories, remain consistent.
PTSD is not only a mental health condition. It is associated with:
> Chronic inflammation that accelerates cellular aging
> Accelerated biological aging as measured by epigenetic clocks
> Increased cardiovascular disease risk
> Higher all-cause mortality (32-47% increased risk according to a 2023 meta-analysis in BMC Psychiatry)
A landmark study published in Neuropsychopharmacology used the GrimAge epigenetic clock to demonstrate that lifetime PTSD is associated with accelerated cellular aging and a shorter predicted lifespan. The researchers found increased cell death in brain regions associated with emotion regulation, changes that persisted even in those whose PTSD symptoms had resolved.
Research from Boston University found that for every year that cells of someone without PTSD age, the cells of someone with severe PTSD symptoms age approximately 1.36 years, a significant acceleration that compounds over decades.
Untreated PTSD can significantly shorten healthspan, making it a longevity issue as much as a psychological one. Understanding the connection between stress and aging is fundamental to grasping why effective PTSD treatment may be a legitimate longevity intervention.
How Psychedelics Affect the Brain (And Why It Matters for Aging)
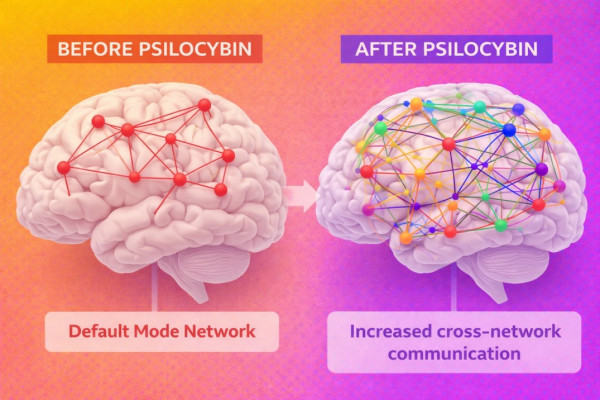
One of the most consistent findings in psychedelic research is increased neuroplasticity. Psychedelics temporarily disrupt rigid neural patterns, allowing the brain to form new connections.
A 2024 study published in Nature tracked healthy adults with precision functional MRI before, during, and for three weeks after psilocybin administration. The findings were striking: psilocybin caused more than threefold greater disruption to functional connectivity than the control compound (methylphenidate), with some changes persisting for weeks.
From an aging perspective, this matters because:
> Cognitive decline is linked to reduced plasticity and neural rigidity
> Neuroplasticity supports learning, emotional regulation, and resilience, all of which decline with age
> Enhanced plasticity may counteract age-related rigidity in thinking and behavior
> The prefrontal cortex and hippocampus, regions critical for memory and executive function, show particular responsiveness to psilocybin's neuroplastic effects
Rather than "damaging" the brain, psychedelics appear to create a window for rewiring, potentially supporting cognitive function and mental flexibility as we age.
Psilocybin and Neuroplasticity
Psilocybin, the active compound in psychedelic mushrooms, has been shown to promote structural and functional changes in the brain. Imaging studies demonstrate increased connectivity between regions that typically do not communicate.
At the molecular level, psilocybin's effects on neuroplasticity are mediated through several key pathways:
> 5-HT2A receptor activation triggers downstream signaling cascades
> BDNF (brain-derived neurotrophic factor) levels increase, supporting neurogenesis
> mTOR pathway activation promotes dendritic spine growth and synaptic remodeling
> Synaptic proteins including PSD-95 and synapsin-1 show elevated expression
A 2024 systematic review examining psilocybin's cognitive effects found that while global cognitive function remained largely unchanged in healthy individuals, patients with treatment-resistant depression showed improvements in sustained attention, working memory, and executive function, domains particularly vulnerable to aging.
In clinical trials, these changes correlate with sustained improvements in depression, anxiety, and emotional openness, sometimes lasting months after a single session. While not proven to extend lifespan directly, preserving cognitive flexibility is a core pillar of mental longevity.
For those interested in measuring their own biological aging, epigenetic age tests and understanding epigenetic clocks offer concrete tools for tracking progress.
Psychedelic Therapy and Veterans With PTSD
One of the most compelling bodies of evidence comes from studies involving combat veterans. Trials using compounds such as MDMA, ketamine, ibogaine, and 5-MeO-DMT have produced dramatic reductions in PTSD symptoms, suicidal ideation, and depression.
The COMPASS Pathways Phase 2 study (results published January 2025) demonstrated that a single 25mg dose of psilocybin produced rapid and durable symptom improvement in PTSD patients across sites in the UK and US, with benefits maintained through the 12-week follow-up period.
Participants frequently report:
> Long-term symptom remission that persists beyond the drug's presence in the body
> Increased psychological flexibility and openness to new experiences
> Renewed sense of purpose and connection to others
> Reduction in hypervigilance and emotional numbing
These outcomes persist well beyond the acute effects of the drug, suggesting durable neurological and psychological changes. The VA has begun actively soliciting psychedelic research proposals for PTSD and depression treatment, signaling institutional recognition of the therapeutic potential.
Given that PTSD is associated with significantly increased mortality risk, effective treatment represents a legitimate longevity intervention. For veterans and others affected by trauma, working with qualified longevity doctors who understand the mind-body connection may be particularly valuable.
The Mental Health Connection to Lifespan
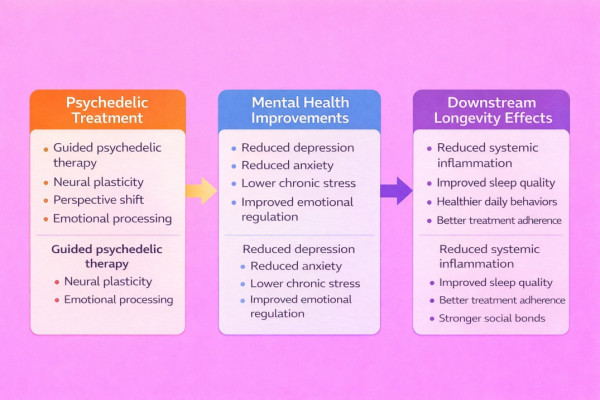
Mental health and longevity are deeply intertwined. Chronic depression, social withdrawal, and psychological rigidity are associated with faster biological aging and higher mortality.
The mechanisms linking mental health to longevity include:
> Chronic inflammation: Depression and PTSD maintain elevated inflammatory markers that accelerate cellular senescence
> HPA axis dysregulation: Sustained cortisol elevation damages multiple organ systems
> Behavioral factors: Mental health conditions reduce adherence to health-promoting behaviors
> Social isolation: Loneliness is associated with mortality risk comparable to smoking 15 cigarettes daily
> Telomere shortening: Chronic psychological stress accelerates telomere attrition
By restoring emotional engagement, curiosity, and adaptability, psychedelics may influence longevity indirectly. A person who regains motivation, connection, and meaning is more likely to:
> Exercise regularly and maintain physical fitness
> Maintain social bonds that protect against cognitive decline
> Adhere to healthy behaviors, including quality sleep
> Avoid destructive coping mechanism,s including substance abuse
> Engage in proactive health monitoring and preventive care
In this way, psychedelics may function as upstream longevity interventions, addressing root causes of health-degrading behaviors rather than treating symptoms. For a comprehensive approach to extending healthy years, see our guide to longevity.
Microdosing for Longevity: Hype or Hope?
Microdosing, taking sub-perceptual doses of psychedelics, has gained popularity as a longevity-adjacent practice. Claims include improved focus, mood, creativity, and cognitive performance.
Scientific evidence remains mixed. A 2024 review of psychedelic effects on cognitive function found that while some studies show modest benefits, others find effects comparable to a placebo. The challenge with microdosing research is significant:
> Expectancy effects are strong, people who believe they're microdosing often report benefits regardless of actual dose
> Dosing protocols vary widely across studies and individual practices
> Long-term effects remain largely unstudied
> Regulatory restrictions limit controlled research
Microdosing is unlikely to produce the profound therapeutic shifts seen in guided psychedelic therapy but may offer incremental cognitive benefits for some individuals. For those interested in cognitive enhancement, established interventions like optimizing sleep and managing inflammation have stronger evidence bases.
The most promising longevity applications of psychedelics likely involve supervised, therapeutic-dose sessions rather than unsupervised microdosing protocols.
Can Psychedelics Help Increase Lifespan?
There is no direct evidence that psychedelics extend human lifespan. However, they may influence factors strongly correlated with longevity:
|
Factor |
Psychedelic Effect |
Longevity Relevance |
|
Chronic stress |
Significant reduction in treatment-resistant cases |
Cortisol drives inflammatory aging |
|
Emotional regulation |
Enhanced flexibility and processing |
Emotional dysregulation linked to CVD, dementia |
|
Cognitive resilience |
Increased neuroplasticity, maintained connectivity |
Cognitive decline predicts mortality |
|
Substance abuse |
Reduction in alcohol and tobacco use disorders |
Major modifiable mortality risk |
|
Social connection |
Increased empathy and relational capacity |
Social isolation is comparable to smoking risk |
|
Depression/anxiety |
Rapid, sustained improvements |
Depression is associated with 40% increased mortality |
Longevity science increasingly recognizes that mental health is not optional, it's foundational. Psychedelics may help preserve the psychological infrastructure required for long life, even if they don't directly target biological aging mechanisms like NAD+ precursors or senolytics.
For those building a comprehensive longevity protocol, addressing mental health may be as important as optimizing biomarkers or implementing heat therapy and cold exposure practices.
Legal Status and Access
Legal access varies widely by region. Some psychedelic therapies are available through clinical trials or specialized clinics, while others remain illegal outside research settings.
Current landscape (as of February 2026):
> Australia: Psilocybin approved for treatment-resistant depression (2023)
> Oregon and Colorado: Legalized psilocybin in supervised therapeutic settings
> Canada (Alberta): Psilocybin available for medicinal purposes in supervised settings
> FDA Status: Psilocybin has breakthrough therapy designation; MDMA application for PTSD was returned for additional study in 2024
> Clinical Trials: Active trials at Johns Hopkins, Mount Sinai, COMPASS Pathways, and others
Regulatory frameworks are evolving rapidly. The FDA issued its first draft guidance on clinical trials with psychedelic drugs in 2024, signaling an effort to standardize research approaches.
Any use should prioritize legality, medical oversight, and evidence-based protocols. Those interested in exploring therapeutic options should work with qualified healthcare providers and consider clinical trial participation where appropriate. Our directory of longevity clinics can help identify practitioners who take an integrative approach to mental and physical health.
Final Perspective
Psychedelics are not longevity drugs. They are mind-level interventions with far-reaching implications for how humans age psychologically.
By restoring adaptability, meaning, and engagement, especially in populations devastated by trauma, they may indirectly extend healthspan. As longevity science matures, it is becoming clear that preserving the mind may be just as important as repairing the body.
Research continues at an accelerating pace. The FDA's breakthrough therapy designations, VA's active solicitation of psychedelic research, and ongoing Phase 3 trials suggest that approved psychedelic therapies may be available within the next few years.
In that sense, psychedelics may not be the fountain of youth, but they could help people remember why living longer is worth it.
Frequently Asked Questions
Do psychedelics make you live longer?
There is no proof of direct lifespan extension from psychedelic use. However, by treating conditions like PTSD and depression, which are associated with 30-50% increased mortality risk, effective psychedelic therapy may indirectly support longevity. The research focus is on mental health improvement, with lifespan benefits as a potential downstream effect.
Do psychedelics slow aging?
Psychedelics may support brain health and stress resilience, which influence biological aging indirectly. Studies show psilocybin increases neuroplasticity and may protect against age-related cognitive rigidity. However, no research has directly measured effects on biological age markers like epigenetic clocks or telomere length following psychedelic treatment.
What drugs increase life expectancy?
No psychedelic has been shown to increase life expectancy in controlled human studies. Most longevity benefits are indirect, through improved mental health, reduced substance abuse, and enhanced social connection. Compounds with more direct evidence for longevity effects include metformin, rapamycin, and NAD+ precursors.
Which mushroom is for longevity?
Psilocybin mushrooms are studied for mental health and neuroplasticity, not direct lifespan extension. For mushrooms with more direct longevity research, lion's mane (cognitive support) and reishi (immune modulation) have established evidence. See our longevity supplements guide for comprehensive coverage.
What is microdosing and does it affect longevity?
Microdosing involves taking very small, sub-perceptual doses of psychedelics (typically 1/10th to 1/20th of a full dose) on a regular schedule. Evidence for longevity benefits is limited and mixed. Most promising psychedelic research involves full therapeutic doses in supervised settings rather than unsupervised microdosing.
How do psychedelics affect brain aging?
Psychedelics increase neuroplasticity and connectivity between brain regions, which may protect against cognitive decline. A 2024 Nature study showed psilocybin produces more than threefold greater functional connectivity changes than control compounds, with some effects persisting for weeks. These changes may counteract the neural rigidity associated with aging.
Are psychedelics legal for longevity purposes?
Generally no. Most therapeutic use is restricted to clinical or research settings. Oregon and Colorado allow supervised psilocybin therapy; Australia has approved it for treatment-resistant depression. Longevity-specific applications are not currently a recognized medical indication. Check local regulations and consider clinical trial participation for legal access.
What does the research say about psilocybin and aging?
Research supports mental health benefits and neuroplasticity enhancement, not direct anti-aging effects. Ongoing trials at Johns Hopkins are examining psilocybin in patients with mild cognitive impairment and early Alzheimer's disease. Published studies demonstrate sustained improvements in depression and anxiety that may support cognitive health long-term.
For more on the connection between mental health and longevity, explore our articles on stress and aging, sleep optimization, and finding your longevity tribe.
About the Author
Sign Up For Our Newsletter
Weekly insights into the future of longevity
