Regenerative Medicine vs Surgery: What Works?

Regenerative Medicine vs Surgery: Do You Need an Operation?
A lot of chronic joint and spine issues are less “broken part” and more “broken signaling,” where inflammation and poor tissue communication block repair. Regenerative medicine tries to restart healing with tools like PRP, imaging-guided injections, and carefully selected biologics, but quality varies and regulation matters. The win is matching the right tool to the right tissue at the right time, and knowing when surgery is still the smartest move.
Why surgery became Plan A (and why that’s changing)
For decades, the script was simple: pain shows up, an MRI looks ugly, and you get moved toward a procedure. Replace the joint. Fuse the spine. Trim the meniscus. To be clear, surgery can be life-changing when it’s the right fit.
The problem is that surgery became Plan A too early for too many people.
Here’s the quieter truth: healing is largely a communication problem. Your body is rarely “out of parts.” It’s often out of the right signals to coordinate repair, calm inflammation, restore function, and rebuild tissue architecture.
That’s the core idea behind regenerative medicine: instead of cutting something out and swapping in hardware, you try to re-activate the body’s repair pathways with targeted interventions plus precision diagnostics.
Once you see it through that lens, the conversation shifts from “What procedure do I need?” to a better question:
What is actually driving my pain, and is this a signal problem, a structure problem, or both?
What does “better signaling” actually mean?
When people say “regenerative,” they often picture something dramatic: regrowing cartilage overnight or reversing arthritis in a month.
That’s not the real promise.
The more realistic promise is this: some interventions can improve the environment around injured tissue, so your body can do what it already knows how to do, repair and adapt.
“Better signaling” usually means:
> Less inflammatory noise
> More coordinated tissue remodeling
> Improved load tolerance through rehab
> Better targeting through diagnostics (and not guessing)
And yes, sometimes, it means avoiding surgery. Other times, it means delaying surgery until it’s truly needed, or making surgery more successful because the tissue is in a better state going in.
Does PRP actually work for knee osteoarthritis?
PRP (platelet-rich plasma) is one of the best-known regenerative tools because it’s using your own blood components to deliver a concentrated “repair team” to a joint or tendon.
For knee osteoarthritis, there’s a growing evidence base showing PRP can improve pain and function for some patients, often comparing favorably to certain conventional injectables, but outcomes vary significantly by:
> PRP preparation method
> OA severity and phenotype
> Dosing schedule and injection technique
> Patient expectations and rehab follow-through PubMed
Here’s the honest takeaway:
> PRP is not “snake oil.”
> PRP is not “guaranteed.”
> PRP is a tool that can work well when you match the right protocol to the right patient.
If you want a “no hype” way to think about PRP: it can be a wake-up signal. It does not rebuild a joint by itself. It can help create conditions where rebuilding is more likely, especially when the mechanical plan (strength, mobility, gait, load management) is handled correctly.
What MRI pain actually means: bone marrow lesions and the subchondral story
One reason people get rushed into surgery is that imaging is often treated like a verdict.
But MRI findings are messy.
Research on MRI features in osteoarthritis shows that bone marrow lesions (BMLs), synovitis, and effusion correlate with pain more consistently than cartilage appearance alone. PubMed and broader evidence suggest BMLs and other MRI-detected features can be associated with progression in knee OA.
Why does this matter?
Because it helps explain why “treat the cartilage” is sometimes the wrong target. If the inflamed bone-cartilage interface (subchondral bone plus the surrounding inflammatory environment) is driving symptoms, then:
> better imaging interpretation matters
> injection placement matters
> load strategy matters
> generic one-size protocols fail more often
This is also where high-quality imaging becomes the boring superpower. A strong diagnostic workup can clarify whether you’re dealing with inflammatory bone changes, cartilage loss patterns, meniscal pathology, tendinopathy, or something else entirely, and that should dictate the least invasive credible option first.
Exosomes and extracellular vesicles: what’s promising vs what’s premature
Now we hit the loudest marketing corner of the room.
“Exosomes” and “extracellular vesicles” (EVs) are being investigated for their ability to influence signaling and tissue behavior. Research is active, including directions in osteoarthritis and regenerative applications.
But here’s the problem: consumer marketing is miles ahead of standard-of-care medicine.
The FDA has issued a public safety notification warning that many exosome products marketed for a wide range of conditions are unapproved and may pose risks, and clinics should not present investigational therapies as guaranteed or routine.
Translation:
> The science is interesting.
> The market is chaotic.
> Promises of certainty are a red flag.
If you are evaluating a clinic offering exosomes:
> Ask what the product actually is, where it comes from, and what oversight exists.
> Ask what outcomes they track.
> Ask what happens if you worsen.
> Be wary of “works for everyone” pitch decks.
Peptides for injury repair: why the hype outpaces the evidence
Peptides are the internet’s favorite shortcut. People want “targeted repair in a vial.” I get it.
But the reality is:
> Human evidence is mixed or limited for many popular compounds
> Quality control and sourcing vary widely
> “Miracle claims” are usually a warning sign, not a feature
The smartest posture here is not “never peptides.” It’s evidence-first, safety-first, clinician-guided. If a clinic is using peptides as part of a broader plan, that can be reasonable. If peptides are being sold as a standalone replacement for diagnosis and rehab, you’re in marketing land.
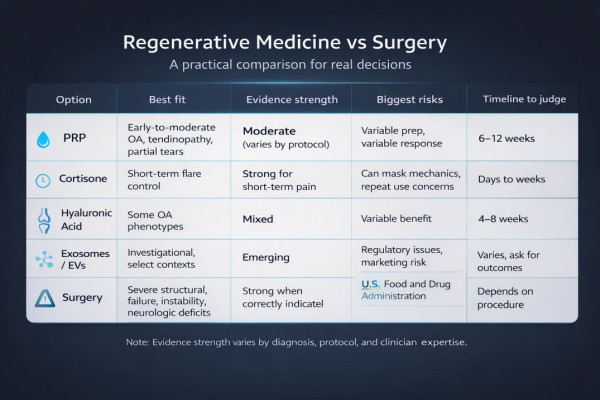
Regenerative medicine vs surgery: a comparison that actually helps
Here’s a practical comparison lens. This is not medical advice, it’s decision support.
Quick comparison table
When should you choose surgery instead? Red flags and timelines
This is the section that builds trust because it tells readers you’re not trying to sell “regen for everyone.”
Consider a surgery-first consult sooner if you have:
> Progressive weakness, numbness, bowel/bladder changes (spine red flags)
> Mechanical locking of a knee
> Severe instability (giving way repeatedly)
> Suspected fracture, infection, tumor, or major neurologic symptoms
> Rapid decline in function despite appropriate conservative care
Also, timing matters. If you wait until the system is severely degenerated, the “signal” tools often have less to work with. Earlier-stage issues generally have more biological flexibility.
How to vet a regenerative clinic: a no-BS checklist
If you want the benefits of regenerative medicine without stepping into hype, use this checklist.
Green flags
> Clear diagnosis and explanation of pain drivers (not just “your MRI is bad”)
> Imaging that matches the plan (and injection guidance when appropriate)
> Transparent discussion of evidence and uncertainty
> Realistic claims with success rates, not guarantees
> Rehab plan is part of the protocol, not an afterthought
> Clear informed consent and adverse event protocols
Red flags
> “This works for everyone.”
> “We regrow cartilage 100% of the time.”
> No imaging standards, no guidance, no measurable outcomes
> Bundled packages sold before diagnosis
> Dismissing surgery as always “bad” (that’s a tell)
Step-by-step: how to start making a smarter decision this week
If you’re trying to decide between surgery and regenerative options, don’t start with the procedure. Start with a process.
Clarify the driver
Is this inflammation-driven pain, mechanical failure, or both?
Get the right imaging and interpretation
Not just “MRI: abnormal.” You want “what abnormality is causing symptoms?”
Match the tool to the tissue
PRP protocols for tendons and OA are not interchangeable. Neither are injection sites.
Build the operating system
Protein sufficiency, strength training that respects tissue capacity, sleep, and inflammation control.
These are not “nice-to-haves.” They are the platform your interventions run on.
Set a timeline with pivot points
If you see no meaningful progress by an agreed checkpoint, reassess.
Explore options with qualified clinicians
If you want to explore credible options with qualified clinicians, start here and compare approaches:
Find a doctor: https://spannr.com/articles/longevity-doctors
Location guide: https://spannr.com/articles/longevity-doctors-los-angeles
What’s next: better diagnostics, clearer standards, smarter timing
This is where 2025 and beyond gets interesting: better diagnostics, more precise delivery, and hopefully clearer standards.
The future is not “everyone gets exosomes.”
The future is:
> identify the real bottleneck (signal vs structure vs mechanics)
> confirm it with the right imaging and history
> apply the least invasive intervention that has credible evidence for that pattern
> escalate only when it’s warranted
If you want the deeper nuance and clinician-grade protocols from someone living in this world every day, listen to the full conversation with Dr. Jeff Gross (former neurosurgeon turned regenerative medicine specialist). We get into what actually changes outcomes, what imaging standards should look like, and why the “surgery-first” default is starting to feel outdated.
In Closing (from Brent)
For a long time, I treated surgery like the end of the story. Pain shows up, scan looks ugly, procedure happens, the end.
Now I see it differently. A lot of what we call “damage” is a system stuck in the wrong conversation: too much inflammation, too little capacity, poor diagnostics, and a one-size plan.
Regenerative medicine is not magic. But it is a smarter question: can we change the signal before we replace the parts?
Sometimes the answer is yes. Sometimes the answer is still surgery. The win is choosing based on evidence, timing, and reality, not fear, marketing, or default pathways.
Cheers,
Brent and the Spannr Team
FAQs about Regenerative Medicine
Is regenerative medicine a real alternative to surgery?
Sometimes, especially earlier in the disease process, but outcomes depend on diagnosis, tissue quality, clinician skill, and whether the therapy is evidence-aligned.
Do exosomes regrow cartilage?
Early research is still developing, but consumer claims often outrun clinical standards. Treat “guaranteed regrowth” as marketing, not medicine.
Does PRP work for knee osteoarthritis?
Many studies show PRP can improve pain and function for some patients, but protocols vary widely and not everyone responds.
Are peptides like BPC-157 proven for injury repair?
Human evidence is limited for many popular peptides and quality control can be inconsistent, so risk-benefit should be discussed with a qualified clinician.
How do I know if a clinic is legit?
Look for clear informed consent, realistic claims, appropriate imaging and diagnostics, transparent sourcing, tracked outcomes, and no “one therapy fixes everything” sales pitch.
Disclaimers
Medical disclaimer:
Content is for educational purposes only and is not medical advice. Always consult a qualified healthcare professional before making changes to your health regimen.
Affiliate disclosure:
Spannr may receive compensation when you click partner links and make a purchase. As an Amazon Associate, we earn from qualifying purchases.
HIPAA/PHI notice:
Do not send personal medical information to this inbox. Spannr does not collect or store PHI via email.
About the Author
Sign Up For Our Newsletter
Weekly insights into the future of longevity
